As evidence-based practitioners, your commitment to clinical precision is undeniable. Research, guidelines, and best practices form the foundation of your care.
But here’s a truth that might surprise you: patients aren’t always looking for the studies or the science.
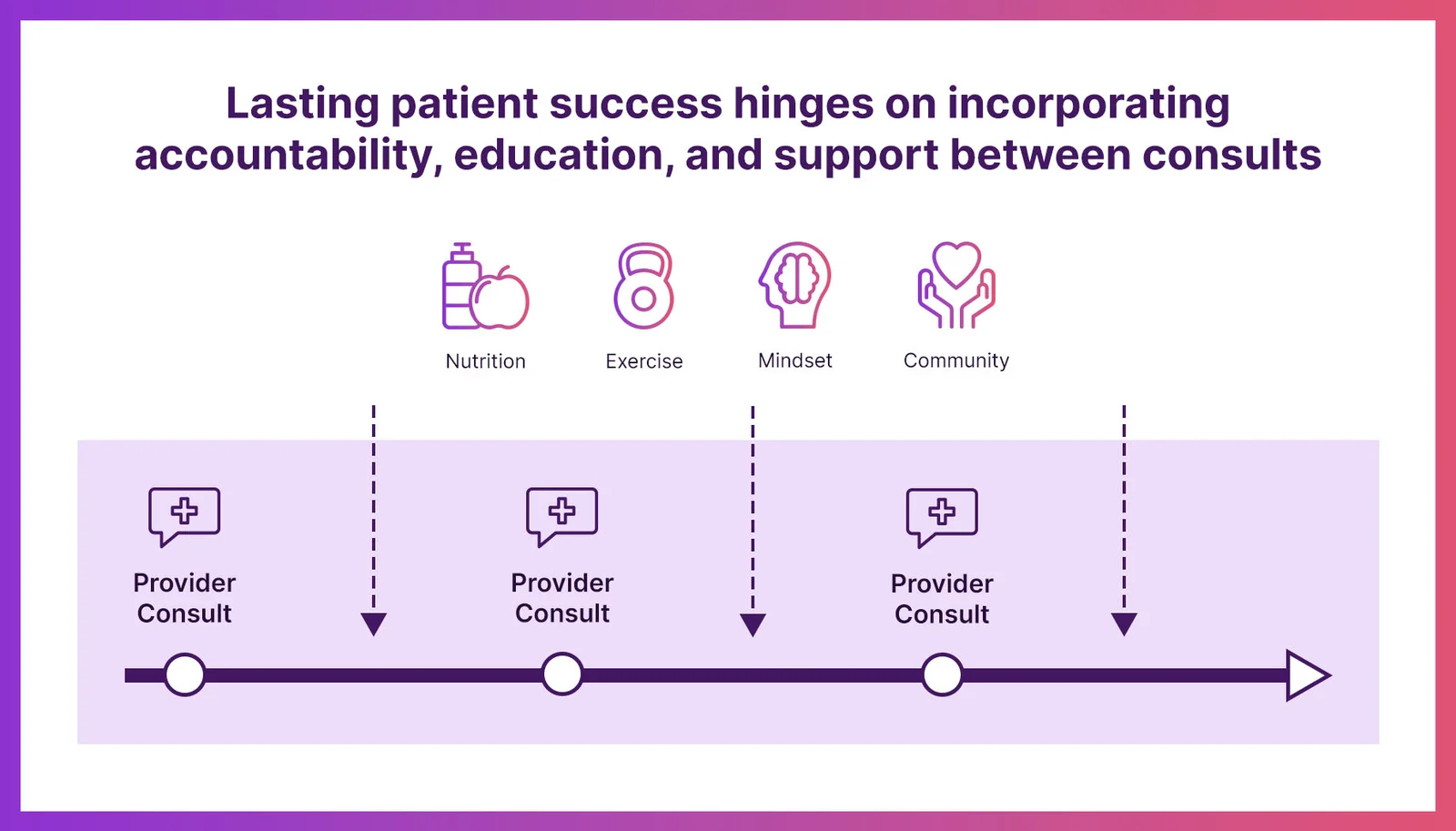
They trust you’ve got that covered. What they crave is something far more personal — accountability, a listening ear, and unwavering support.
In today’s healthcare landscape, success is no longer just about offering the best treatments; it’s about fostering human connection and guiding patients toward real, sustainable habit change. If you’re an evidence-based doctor, here’s why you should rethink how you deliver care and help your patients find the emotional, practical, and holistic support they need to thrive.
The gap between clinical expertise & patient needs.
Patients seek healthcare to feel better, both physically and emotionally. While clinical protocols save lives, they can often feel impersonal to the people sitting in front of you. Your patients want to know you understand their struggles — not just their symptoms.
For many, especially those managing chronic conditions like obesity, diabetes, or hypertension, it’s not the treatment plan itself that’s challenging — it’s sticking to it. They don’t need another pamphlet about the benefits of eating more vegetables or exercising three times a week. What they need is:
– Accountability: Someone to check in with them regularly.
– Empathy: A provider who listens to their unique barriers and concerns.
– Encouragement: Support to get back on track when motivation wanes.
Evidence-based care provides the “what” of treatment, but accountability and support provide the “how.”
The value of well-rounded, collaborative care.
Addressing complex conditions like obesity requires more than medical expertise — it demands a collaborative approach that helps patients achieve meaningful, long-term habit changes. While accountability and emotional support are critical, patients benefit most when care plans encompass the many facets of obesity management:
– Nutrition: Equipping patients with realistic meal plans, education, and tools to make better food choices.
– Exercise: Introducing movement in a way that’s accessible, sustainable, and tailored to individual fitness levels.
– Behavioral health & self-care: Helping patients address emotional eating, build self-compassion, and develop coping mechanisms.
– Mindset: Encouraging a growth-oriented approach that fosters resilience and long-term commitment to health.
When patients experience this kind of holistic, team-based care, they’re more likely to engage with their treatment plans, feel supported, and achieve meaningful progress.
How evidence-based providers can meet these needs.
You don’t have to shoulder the entire burden of support — nor should you. Instead, you can integrate systems and partnerships to ensure your patients receive the accountability and care they need.
1) Build a collaborative care team:
Leverage your staff or collaborate with professionals like health coaches, dietitians, exercise specialists, or counselors. Together, you can address the diverse needs of your patients while reinforcing consistent messaging.
2) Offer community-based support options:
Support groups — whether in-person or virtual — connect patients with others who understand their challenges. Encourage participation in these groups to foster a sense of community and shared accountability.
3) Adopt holistic care platforms:
Consider adopting patient-centered platforms that integrate resources for nutrition, exercise, and behavioral health. These tools can provide patients with ongoing education, check-ins, and tailored recommendations.
4) Focus on habit change over perfection:
Encourage patients to build sustainable habits rather than striving for unattainable ideals. Small, incremental changes in diet, activity, and mindset create lasting transformations over time.
5) Strengthen empathy during visits:
Small shifts in your interactions can make a big difference. Taking five minutes to ask, “What feels hardest for you right now?” can strengthen trust and open the door to meaningful conversations.

A new standard of care.
Evidence-based medicine will always be the backbone of high-quality healthcare. But it’s not the full picture. When you combine your expertise with systems that prioritize accountability, collaboration, and habit change, you’ll not only improve patient outcomes — you’ll build loyalty and trust that lasts a lifetime.
So, the next time you’re crafting a care plan, ask yourself: Does this address the whole patient? Who will help them overcome obstacles and build sustainable habits? If the answer isn’t clear, it’s time to rethink how you deliver support.
Your patients don’t just need evidence; they need a well-rounded, collaborative care team to guide them on their journey. By prioritizing accountability, empathy, and holistic care, you can empower your patients to succeed in ways they never thought possible.
In the face of an escalating obesity crisis, it’s crucial for obesity medicine specialists to recognize the limits of their expertise in areas like nutrition and behavior change. By collaborating with specialized platforms, you can enhance patient care, optimize outcomes, and create a more sustainable practice. Position yourself as a clinic that embraces a comprehensive approach to obesity management — one that supports lasting change for your patients while allowing you to focus on your unique strengths. Together, we can tackle the obesity epidemic more effectively.
❤️ Want to provide even better holistic care for your patients?
Be sure to download our FREE Obesity Medicine Practice Growth Toolkit with video lessons and 5 holistic care tools you can start giving to your patients today!
Did you know Alterra Health provides 360° education and support programs designed to meet the needs of medical weight loss clinics of all sizes?
Let’s chat, and we’ll show you how it works!
We’re happy to have a conversation free of charge with no strings attached, no matter the size of your practice. 🤝

Article by: Whittany Gibson, RDN
Whittany is the Co-Founder of Alterra Health and a seasoned Registered Dietitian specializing in bariatric and medical weight loss. With over ten years of expertise in the weight loss industry, she designs comprehensive nutrition, mindset, exercise, and coaching programs to support patients on their journey to better health.
